By Domenica Angelo & Libby Parker, MS, RD, CDN, CEDS-C
Domenica is currently a graduate student at Thomas Jefferson University in their MS/RDN program. She is excited to gain the tools to become a successful dietitian and wants to make a positive impact on the health and wellness of individuals who struggle/lose their love for food.
Did you spend any significant time learning about eating disorders (ED) in your education? No? You’re not alone. Most medical professionals spend only around one class period learning about EDs, and are supposed to treat this complex population!
It can be tricky to get the best treatment for a patient if you do not know the specific terminology and assessments used by ED specialists. This article will help medical professionals understand this terminology. Understanding what these terms mean can be crucial in any medical setting. This is a chance to educate yourself a little more about disordered eating, treatments, and what values are important to look at when assessing an individual at risk for this mental illness.

Medical / Assessments:
Orthostatic Vitals
Taking blood pressure at two (or three) different positions with specific timing between measurements is how we assess if an individual has orthostatic hypotension (a quick drop in blood pressure). This is done by having the patient’s blood pressure taken while in a supine position, (potentially again while sitting), then asked to stand and measure their blood pressure again. The physician should be additionally asking/making notes about the patient’s dizziness.
Orthostatic hypotension
A condition in which your blood pressure suddenly drops at least 20 points when you stand up from a seated or lying position. Hypotension often presents as dizziness upon sitting or standing and possibly fainting from a quick change in position. This is commonly associated with anorexia nervosa.
Source: U.S. Department of Health and Human Services. (n.d.). Orthostatic hypotension. National Institute of Neurological Disorders and Stroke. https://www.ninds.nih.gov/health-information/disorders/orthostatic-hypotension#:~:text=Orthostatic%20hypotension%20is%20a%20condition,Blurred%20vision
Why are these measurements important to eating disorder specialists?
Orthostatic hypotension is a marker of a weakened cardiovascular system due to starvation. The mechanism that maintains blood pressure is compromised due to the alteration of the autonomic nervous system, which is a result of disordered eating behaviors and should signal a need for intervention.
Source: Graphics, C. (2019, November 25). Orthostatic hypotension-what do I need to know?. Avalon Hills. https://avalonhills.org/orthostatic-hypotension-what-do-i-need-to-know/
Bradycardia
Bradycardia is a slowed heart rate. An average adult’s resting heart rate is between 60 – 100 beats per minute, but with bradycardia, the resting heart rate is less than 60 beats per minute.
Why do eating disorders cause bradycardia?
Anorexia Nervosa (AN) is the restriction of energy intake relative to an individual’s requirements. This eating disorder has a deathly impact on the heart. The restriction of nutrients causes muscles to shrink including the heart. The impact of anorexia nervosa (AN) forces the body to reserve energy because of severe malnourishment, and the body’s response to this is a slow heart rate to conserve the energy that has been lost.
Eating disorders are mental health disorders, while other mental health disorders normally do not affect the physical health of an individual to such an extent, eating disorders can severely damage an individual’s physical state. Anorexia Nervosa has many medical complications and cardiac issues are the most common and are accounted for most deaths. Internally, losing a significant amount of weight in a rapid period causes stress on the heart.
Sources: Mehler, MD, FACP, FAED, CEDS, P. S. (2022, May 1). Bradycardia: How severe is too severe? understanding bradycardia in eating disorders (May 2022).
Robyn L. Goldberg. https://askaboutfood.com/bradycardia-how-severe-is-too-severe-understanding-bradycardia-in-eating-disorders-may-2022/
Strickland, K. (2022, September 22). 6 significant health risks of anorexia nervosa. Walden Eating Disorders. https://www.waldeneatingdisorders.com/blog/6-significant-health-risks-of-anorexia-nervosa/#:~:text=The%20malnutrition%20associated%20with%20anorexia,heart%20rate%20to%20conserve%20energy.
Athlete’s Heart
Patients with anorexia nervosa may indicate their low heart rate as having an “athlete’s heart.” Due to being extremely active, or even an actual athlete, the patient may believe they have the lower heart rate of a conditioned athlete.
These individuals could be working out, but their malnourished/starved heart is not because of their “athletic condition.” If a physician were to ask a patient with severe anorexia nervosa to move, they would show an abnormal heart rate (orthostatic hypotension) just by standing up from a lying position. Additionally, the patient would have a spike in heart rate that a conditioned athlete would not have for the minimal exertion of going from resting to walking a short distance.
“Moreover, ultrasound of the heart in these patients reveals small, thin heart chambers versus a normal chamber size seen in athletes. Unfortunately, few medical providers are well-trained in understanding this issue. The idea of the “athletic heart” is often accepted by healthcare professionals, whereas a trained eating disorder expert would recheck the pulse following minor exertion and recognize that bradycardia — appearing alongside a very low body weight — is a likely indication of anorexia nervosa.”(Mehler, MD, FACP, FAED, CEDS, 2022)
Mehler, MD, FACP, FAED, CEDS, P. S. (2022, May 1). Bradycardia: How severe is too severe? understanding bradycardia in eating disorders (May 2022). Robyn L. Goldberg. https://askaboutfood.com/bradycardia-how-severe-is-too-severe-understanding-bradycardia-in-eating-disorders-may-2022/
Contraindication of hormonal birth control (BC) when an ED client has amenorrhea
An early sign of Anorexia Nervosa (AN) is amenorrhea, which is the absence of menstrual cycles. The result of low food intake or high physical activity disrupts the hypothalamic signals to the pituitary gland, which impacts the menstrual cycle. Since the body is enduring long periods of stress on every organ, another factor the individual with anorexia nervosa might face is a loss of BMD (bone mineral density). “The reason for bone density loss is considered to be related to the low body mass index, a low caloric intake, a low intake of calcium and vitamin D, low estrogen levels, low insulin-like growth factor 1 (IGF-1) levels, and cortisone supplements.” (Bergström et al., 2013)
Physicians began treating patients with AN with estrogen treatment/ birth control to prevent loss of BMD, but in many studies, it was proven that oral therapies can not repair or prevent low BMD as improved nutrition is the most important factor for bone health in patients. In the studies, they all concluded that the lack of effect of estrogen on bone density is depressing the IGF-1 levels even more. Although there is a lot of evidence that hormone treatment does not prevent a loss of BMD, many clinicians still prescribe birth control to their patients, because of the induced menstrual cycles on the week “off.” These cycles give a false sense of health because they are masking the underlying issue.
Bergström, I., Crisby, M., Engström, A.-M., Hölcke, M., Fored, M., Kruse, P. J., & Sandberg, A.-M. (2013, May 20). Women with anorexia nervosa should not be treated with estrogen or … https://obgyn.onlinelibrary.wiley.com/doi/10.1111/aogs.12178
DEXA z/t-scores
The DEXA (Dual-Energy X-Ray Absorptiometry) score tests for an individual’s bone density, which is used to determine whether an individual has healthy bone density, osteopenia or osteoporosis.
For those ages 20-50, Z-scores less than -2 indicate low bone mineral density for age.
For those older than 50, T-scores between -1 and -2.5 denote osteopenia. Anything lower than -2.5 denotes osteoporosis.
Bone Health & Eating Disorders. Home – InsideOut Institute. (n.d.). https://insideoutinstitute.org.au/resource-library/bone-health-eating-disorders#:~:text=The%20DEXA%20scan%20generates%20a,(Robinson%20et%20al%202019)
Why are these scores important regarding disordered eating?
These scores show decreased bone mineral density and strength as the eating disorder progresses. Weight is the most consistent predictor of BMD at all skeletal sites (Grinspoon et al, 2000), associating Anorexia Nervosa with low bone mineral density and an increased risk of fracture (Fazeli & Klibanski, 2018). There is a correlation in both males and females between low body weight and low bone mineral density.
Bone Health & Eating Disorders. Home – InsideOut Institute. (n.d.). https://insideoutinstitute.org.au/resource-library/bone-health-eating-disorders#:~:text=The%20DEXA%20scan%20generates%20a,(Robinson%20et%20al%202019)
Blind Weight
A blind weight is when the patient is unable to see, or know, their weight. Often the provider will ask the patient to step on the scale backward so they are not facing the values, or using a scale that the provider can see the weight but the patient cannot.
Why is this important?
Most individuals with this illness put a high value on the number on the scale, and strive to be a specific number or to have some sort of control. This number can also be a trigger for the eating disorder to resurface or intensify. The importance of taking a blind weight, and not telling the patient any descriptors of their weight can be beneficial to their recovery because the number on the scale is something that can alter their behaviors and consume their thoughts. By taking a blind weight it allows them to be able to engage more in their recovery. Because of the societal pressure on body size, blind weights can be beneficial to most patients that come through your doors, ED or not.
Wood, C. (2023, February 23). What is a blind weight?. Christine Wood MD. https://www.christinewoodmd.com/post/what-is-a-blind-weight
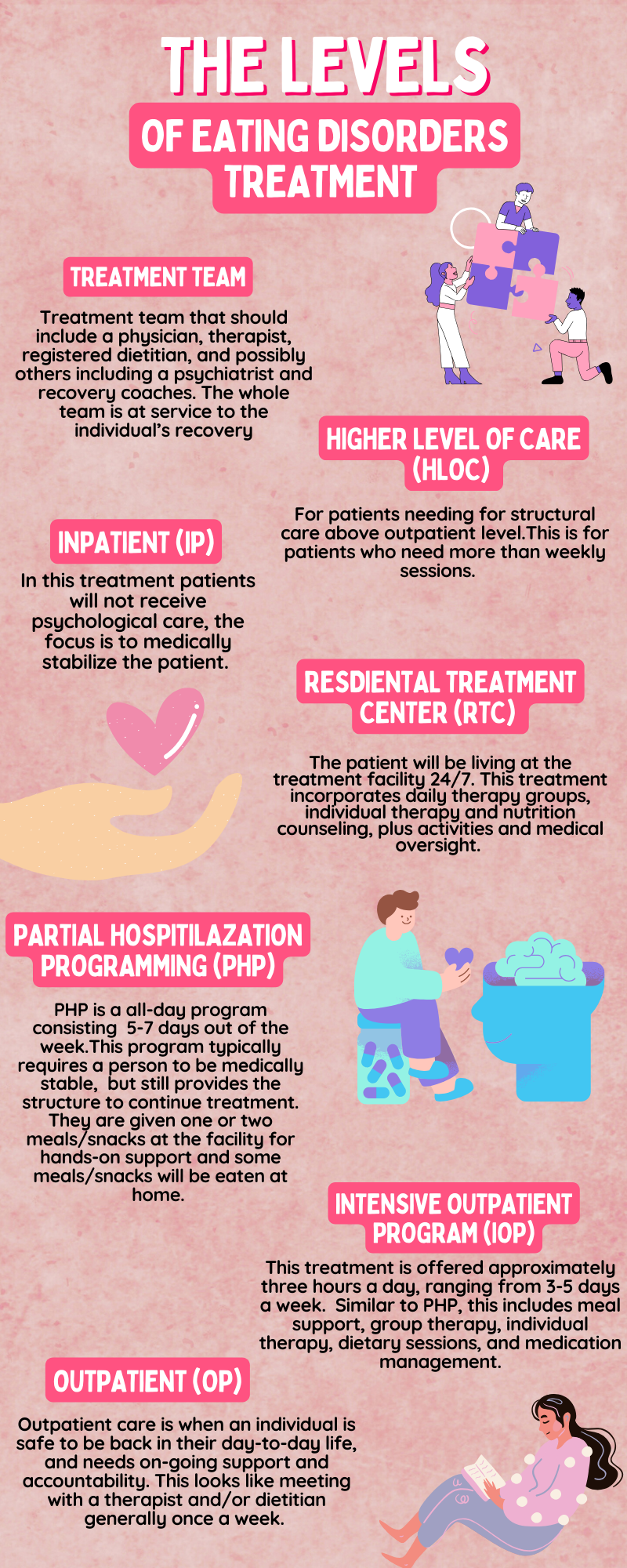
Levels of Treatment:
Higher Level of Care (HLOC)
There is a hierarchy to disordered eating treatment. A HLOC is indicated for patients needing more than weekly sessions with eating disorder professionals, and referring to anything above outpatient level care. HLOC is for patients with more severe functional impairment and symptoms. HLOCs provide a safe and structured environment for patients who are dealing with these life-threatening disorders.
Anderson, L. K., Reilly, E. E., Berner, L., Wierenga, C. E., Jones, M. D., Brown, T. A., Kaye, W. H., & Cusack, A. (2017, June 27). Treating eating disorders at higher levels of care: Overview and challenges – current psychiatry reports. SpringerLink. https://link.springer.com/article/10.1007/s11920-017-0796-4
Outpatient (OP)
Outpatient care is the lowest level of care / least intensive. On a basic level, the individual will be seeing a dietitian, therapist, and possibly others on their treatment team on a regular (typically weekly) basis. Outpatient treatment may include other providers including psychiatrists, recovery coaches, and others. They should also be seeing their primary care provider on a regular basis (frequency depending on the needs of the individual).
Intensive Outpatient Program (IOP)
This treatment is offered approximately three hours a day ranging from 3-5 days a week. This type of program will best suit patients who are ready to be more independent in their lives. IOP typically includes meal support, group therapy, individual therapy, dietary sessions, and medication management. Many programs offer both in-person and virtual options of IOP.
Partial Hospitalization Programming (PHP)
A step up from IOP, PHP is offered 6-8 hours a day five to six days a week. This is for individuals who need more supervision to complete their meals and avoid using behaviors. In these sessions, patients are still receiving individual and group therapy, meal support, nutritional counseling, and medical monitoring.
Simpson, C. C., Towne, T. L., Karam, A. M., Donahue, J. M., Hadjeasgari, C. F., Rockwell, R., & Kaye, W. H. (2021). Predictors of Stepping Up to Higher Level of Care Among Eating Disorder Patients in a Partial Hospitalization Program. Frontiers in psychology, 12, 667868. https://doi.org/10.3389/fpsyg.2021.667868
Residential Treatment Center (RTC)
The patient will be living at the treatment facility 24/7 for often for a month or longer, depending on the client. This treatment incorporates the same services as IOP and PHP, plus more activities and greater medical oversight. The benefit of residential is the around-the-clock supervision to ensure safety and break behavioral patterns. It is ideal for a client to step down to PHP and/or IOP following their stay at RTC. To help them integrate back into “real life.”
Inpatient hospitalization
Is designed for eating disorder patients with medical instability. In this form of treatment, patients will not receive much, if any, psychological care, the focus is to medically stabilize the patient. This may include IV fluids, tube feeding, TPN (IV nutrition), and other medical procedures. Patients will be monitored for cardiac complications and refeeding syndrome.
Treatment Team
In the great majority of eating disorder cases, there is a need for a specialized treatment team. Because eating disorders are complex illnesses involving both the brain and the body, the team may include a primary care physician, an individual therapist, a registered dietitian, a psychiatrist, and a family therapist. The treatment must work collaboratively and communicate to give the best service to the individual.
Ideally, all of these team members are highly experienced and specialized in the treatment of eating disorders. Finding these providers is something The Broadway Dietitian can help with at all levels of care.
Eating disorder treatment team: Alliance for Eating Disorders Awareness. National Alliance for Eating Disorders. (2023, July 10). https://www.allianceforeatingdisorders.com/members-of-treatment-team/
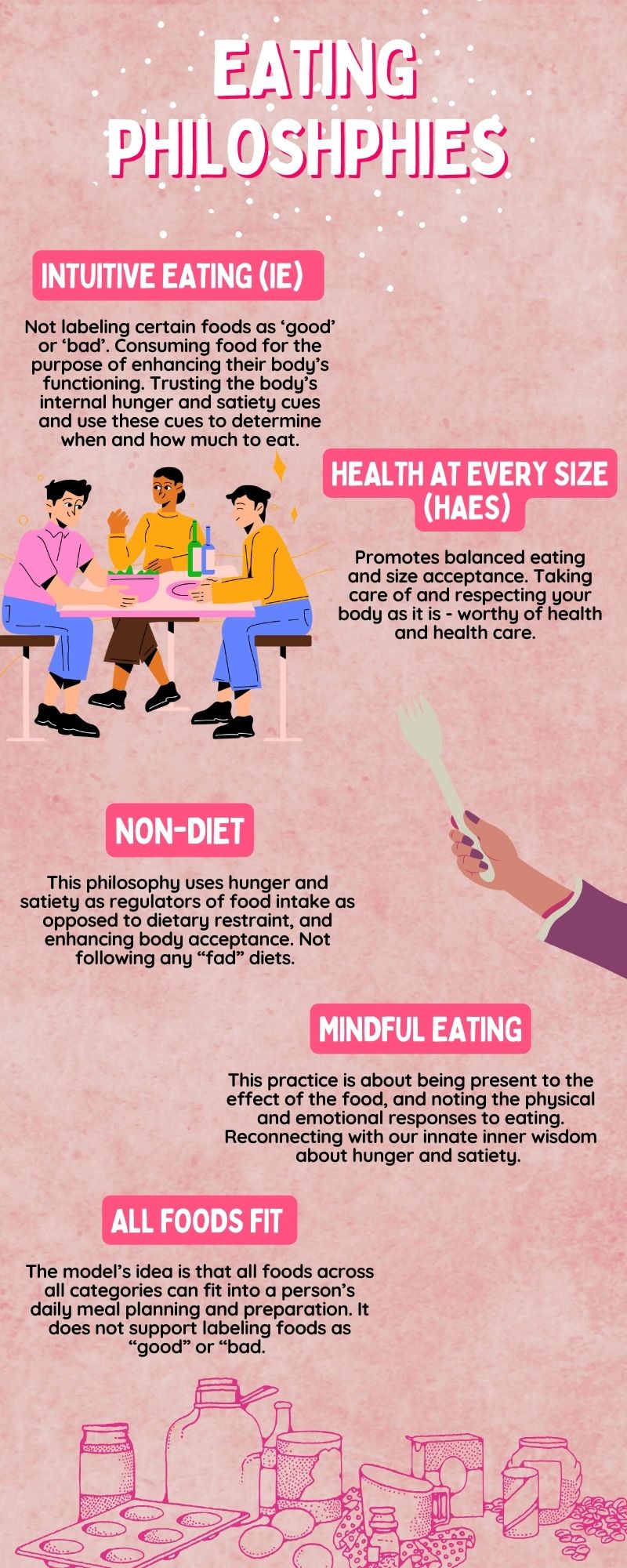
Treatment Philosophies
Intuitive Eating (IE)
Popularized by dietitian authors Evelyn Tribole, and Elyse Resch, Intuitive Eating is, “an adaptive form of eating characterized by a strong connection with internal physiological hunger and satiety cues. Those who eat intuitively are not preoccupied with food or dieting and do not label certain foods as ‘good’ or ‘bad’. The goal of intuitive eating is to reconnect our nature of listening to our cues of when we are hungry or full. Intuitive eating is mainly about trusting our bodies, because they will signal what is needed to fulfill our needs.”
Mauldin, K., May, M., & Clifford, D. (2022). The consequences of a weight-centric approach to healthcare: A case for a paradigm shift in how clinicians address body weight. Nutrition in clinical practice : official publication of the American Society for Parenteral and Enteral Nutrition, 37(6), 1291–1306. https://doi.org/10.1002/ncp.10885
Health at Every SizeⓇ (HAES)
This principle focuses on health not weight. The approach of HAES is to have confidence in every body, whether that is a larger or smaller body. HAES focuses on not using weight as a measurement for health because there are so many other factors to determine the health status of an individual. This approach strives for all individuals to enjoy a healthy-lifestyle, and to have access and dignity in healthcare. HAES focus is to allow people to trust their bodies and what needs their body is signaling.
In a nutshell, HAES is “A paradigm that supports “size- acceptance, to end weight discrimination, and to lessen the cultural obsession with weight loss and thinness” promotes “balanced eating, life-enhancing physical activity, and respect for the diversity of body shapes and sizes.”
Mauldin, K., May, M., & Clifford, D. (2022). The consequences of a weight-centric approach to healthcare: A case for a paradigm shift in how clinicians address body weight. Nutrition in clinical practice : official publication of the American Society for Parenteral and Enteral Nutrition, 37(6), 1291–1306. https://doi.org/10.1002/ncp.10885
Non-Diet
The Non-Diet approach rejects diet culture/fad diets because they are typically too restrictive, and do not last long term. In fact, research shows that 95% of diets fail. By fail we mean the person cannot maintain the diet, and gains the weight back (usually plus some). This causes dieters to be on an un-ending cycle of dietitng, failing, and dieting again, leaving them defeated and unmotivated. Dieting is also the #1 precursor to developing an eating disorder.
Instead of that, the Non-Diet approach focuses on healthy long-term habits. This is a “diet” that has no restrictions, and allows an individual to have freedom over an eating pattern.
This approach, “emphasizes “eating in response to physiological dues, i.e. using hunger and satiety as regulators of food intake as opposed to dietary restraint, and enhancing body acceptance, regardless of whether an individual is successful at weight control.”
Mauldin, K., May, M., & Clifford, D. (2022). The consequences of a weight-centric approach to healthcare: A case for a paradigm shift in how clinicians address body weight. Nutrition in clinical practice : official publication of the American Society for Parenteral and Enteral Nutrition, 37(6), 1291–1306. https://doi.org/10.1002/ncp.10885
PhD, J. C. (2022, February 1). Why diets often don’t lead to long-term weight loss – what to focus on instead: Ohio State Health & Discovery. Ohio State Health and Discovery. https://health.osu.edu/wellness/exercise-and-nutrition/that-diet-probably-did-not-work#:~:text=According%20to%20the%20latest%20weight,people%20maintain%20that%20weight%20loss.
Mindful eating
Mindful eating is relying on the body’s senses and to have the freedom to have any food choice to their desire in moderation. The term mindfulness means to be paying attention, and being present within the moment. In simple terms, mindful eating is an approach to pay more attention to the different emotions of food. By focusing on the difference between physical and emotional hunger the individual can acknowledge the emotions around food instead of judging the feelings. This approach allows the individual to become more attuned with their body, because this principle is not built on strict rules.
“An approach to eating that supports becoming aware of “thoughts, feelings, and physical sensations related to eating, reconnecting with our innate inner wisdom about hunger and satiety.” It is conceptualized as “being aware of the present moment when one is eating, paying close attention to the effect of the food on the senses, and noting the physical and emotional sensations in response to eating.”
Mauldin, K., May, M., & Clifford, D. (2022). The consequences of a weight-centric approach to healthcare: A case for a paradigm shift in how clinicians address body weight. Nutrition in clinical practice : official publication of the American Society for Parenteral and Enteral Nutrition, 37(6), 1291–1306. https://doi.org/10.1002/ncp.10885
Robinson, L. (2023, March 1). Mindful eating. HelpGuide.org. https://www.helpguide.org/articles/diets/mindful-eating.htm
Nelson J. B. (2017). Mindful Eating: The Art of Presence While You Eat. Diabetes spectrum : a publication of the American Diabetes Association, 30(3), 171–174. https://doi.org/10.2337/ds17-0015
All Foods Fit
The All Foods Fit Model is the idea that all foods can fit into a person’s daily meal planning and preparation. The model does not support the idea of categorizing foods into black or white categories–such as labeling foods as “good” vs. “bad” or “healthy” vs. “unhealthy.” The model does not support engaging in fad or elimination diets, and “legalizes” all foods that the individual is not allergic to.
Dmckenzie. (2022, May 18). The all foods fit model to prevent disordered eating < marvelous minds. Marvelous Minds. https://www.marvelousminds.net/prevent-disordered-eating/
This blog was just a glimpse of knowledge as to what eating disorder specialists know. As stated earlier in this blog, many of us are not educated on the many layers involving eating disorders. It is such a complex mental illness and the specialists are here to help! Understanding just a few of the different terms, treatments, and additional knowledge about eating disorders can help specialists give a patient/client a step to recovery even sooner!
The purpose of this blog is to give more awareness to make an impact on those affected by this complex mental illness. Eating disorders can be brought to remission and prevented with the right treatment and knowledge!!
If you need help finding appropriate treatment for yourself, or a client – please reach out! I offer consultation and education to other healthcare professionals, as well.